Fondecyt Regular (2012-2015). Dr. Marcelo Ezquer, investigador responsable.
Diabetes mellitus (DM) is one of the current main threats to public health. The total number of people with either autoimmune (type 1) or insulin-resistance (type 2) DM is projected to rise to 439 million in 2030. The most detrimental complication of both types of DM is diabetic nephropathy (DN), a clinical syndrome comprised of kidney damage and increased risk for cardiovascular disease. Irrespective of DM etiology, the main promoting factors of DN are renal (i) oxidative stress, (ii) chronic inflammation and (iii) accumulation of advanced glycation end products. Moreover, in individuals with DN derived from type 2 DM secondary to obesity, arthrosclerosis and lipids increase into kidneys also seems to play a role in DN progression. Once triggered, DN kidney damage follows a well-known physiopathological course. Microalbuminuria (low levels of urinary albumin excretion) is the earliest detectable sings. It associates with histological changes that include glomerular basement membrane thickening, glomerular mesangial expansion and extracellular matrix deposition. Later on appears macroalbuminuria, followed by a progressive declining of glomerular filtration rate. At this stage, histological changes include the loss of glomerular podocytes, glomerulosclerosis, arteriolar hyalinosis and tubulointerstitial fibrosis. Up to date the handling of people with DN focuses on the control of hyperglycemia and high blood pressure. Still, a significant number of patients require hemodialysis or even kidney transplantation. Therefore, the need for strategies to prevent, delay or revert DN is compelling.
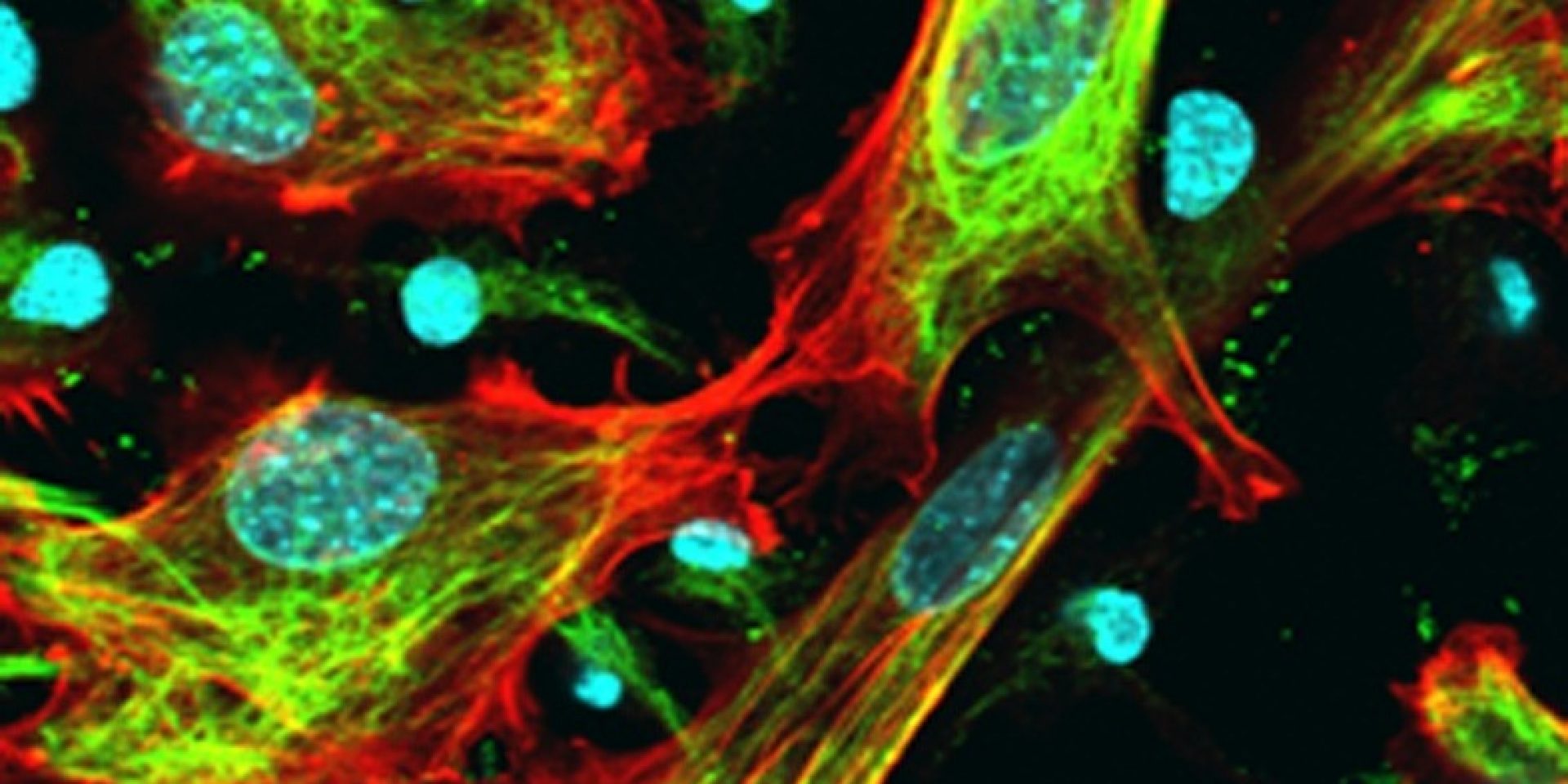
Multipotent mesenchymal stromal cells also referred as mesenchymal stem cells (MSCs) are one of the most promising tool to manage DN progression, not only because they can be safely transplanted in human patients but also due to their proved renoprotective potential. The later, has been attributed to the capacity of MSCs to (i) reduce oxidative stress, (ii) modulate chronic inflammation and macrophage infiltration, (iii) avoid/revert fibrosis, (iv) secrete trophic factors, and (v) differentiate into pericytes, mesangial and tubular cells. Recently, we have shown that the intravenous administration of MSCs into mice with DN derived from type 1 DM, even when hyperglycemia remains uncorrected, prevents kidney damage.
At present, our research aims are to evaluate whether the MSC renoprotective effect depends on DM etiology (type 1 vs type 2) and/or DN stage (early vs advanced). Also, we wonder to study cellular and molecular features expected to be directly modified by donor MSCs in the kidneys of diabetic mice. This, in order to approach to the identification of critical turning points of DN, and whether MSCs modify them. We propose to use mice with DN derived from type 1 DM (DN-T1DM), mice with DN derived from type 2 DM (DN-T2DM) and mice with DN derived from type 2 DM at an advanced stage (advanced DN-T2DM). The animals will receive a single intravenous dose of 0.5 x 106 syngeneic MSCs (MSC-treated) or the vehicle (untreated). For the first two groups the intervention will be performed when the pro-damage mechanisms of DN were already present but kidney structure and function were unaffected. The third group will be intervened when histopathological changes and macroalbuminuria were evidenced. Zero, 5, 10 and 15 weeks after intervention, we will assess (i) renal function (urinary albumin excretion, glomerular filtration rate); (ii) renal structure (histology); (iii) donor cell engraftment into the kidney (flow cytometry and immunohistofluorescence (IHF)); (iv) levels of reactive oxygen species, lipid peroxidation, protein nitrosylation and DNA oxidation (enzymatic assays, IHF); (v) production of pro- and anti-inflammatory cytokines (qRT-PCR and protein arrays) and renal macrophage infiltration (IHF); (vi) apoptosis, proliferation and neovasculogenesis rate (IHF); (vii) production of trophic factors: antiapoptotic, mitotic and vasculogenic (qRT-PCR and protein arrays), and (viii) donor cell differentiation into renal cells (IHF). Data collected will be compared among untreated, MSCtreated and normal (non diabetic age-matched) mice for each animal model. Renoprotection will be concluded if MSC-treated animals in DN-T1DM and DN-T2DM groups did not or delay it progression to DN, and in advanced DN-T2DM group if DN was delayed or reverted.
In view of the match between DN pathologic mechanisms and MSC regenerative potentials we expect that, irrespective of DM etiology and DN stage, MSC administration will be renoprotective in diabetic mice. Regarding to the turning points and the mechanisms we cannot predict which one will be the most critical.
Our preclinical data would be useful to support and refine the design of clinical trials to evaluate MSC-based strategies aimed to prevent, delay or revert DN.